Top industry executives BJ Moore, Executive Vice President and Chief Information Officer, Providence St. Joseph Health; Dr. Ali Parsa, Chief Executive Officer, Babylon Health; and Lucia Savage, Chief Privacy and Regulatory Officer, Omada Health, discussed the evolving doctor-patient relationship and the digitized data and technology convergence with healthcare delivery and payment along with moderators Dale C. Van Demark, Partner, McDermott Will & Emery; Rachel S. Hall, Partner, Digital Health Leader, EY; Stephen W. Bernstein, Partner, McDermott Will & Emery; and Lisa Schmitz Mazur, Partner, McDermott Will & Emery. They also provided insight into 2021’s regulatory considerations affecting healthcare innovation and its solutions.
Below are the top takeaways for McDermott Will & Emery and EY during the 2021 J.P. Morgan Healthcare Conference: Digital Health Pioneers Forum, click here to access the full webinar.
Access the PDF here.
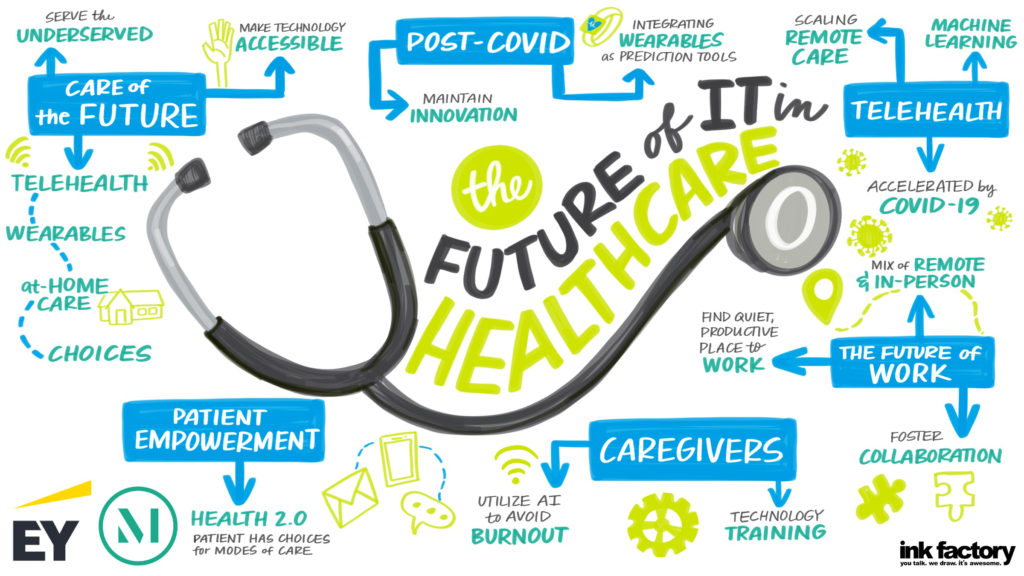
CARE OF THE FUTURE
We are only seeing the beginning of the decentralization of care through information technology; but that shift is how scalable solutions to our health care challenges will develop. “Care delivery at home, where we can send patients home and remotely monitor them—eventually that will evolve to things like wearables -IoT devices- that we may have in our clinical settings. We’re seeing the hospitals play such a critical role during COVID-19, but what’s also been even more apparent as these alternative means of delivery develop is really how we’re going to scale and change the patient experience and ultimately improve the patient outcome,” BJ Moore, executive vice president and chief information officer at Providence St. Joseph Health, said.
PATIENT EMPOWERMENT AND REDUCING CAREGIVER BURNOUT
“By putting that patient in the center, giving them multiple modes of care and allowing that patient to select those modes of care, it ultimately improves that patient experience. But we also recognize it can’t all be on the patient’s shoulders,” BJ Moore said. Nor can we simply burden the provider community with more data and more tasks and expect the promise of digital tools to be achieved. BJ Moore continues, “It’s probably our single biggest issue in healthcare: caregiver burnout and caregivers overwhelmed. We see that as an issue. There’s more help that we need to deliver for the caregivers. Right now, if you look at technology and healthcare, from my opinion, one plus one equals one. And really what it should be is technology should be a force multiplier; what our caregivers put in, that one plus one should equal 10. They should feel like they get a lot more out of the systems (than) they put in.”
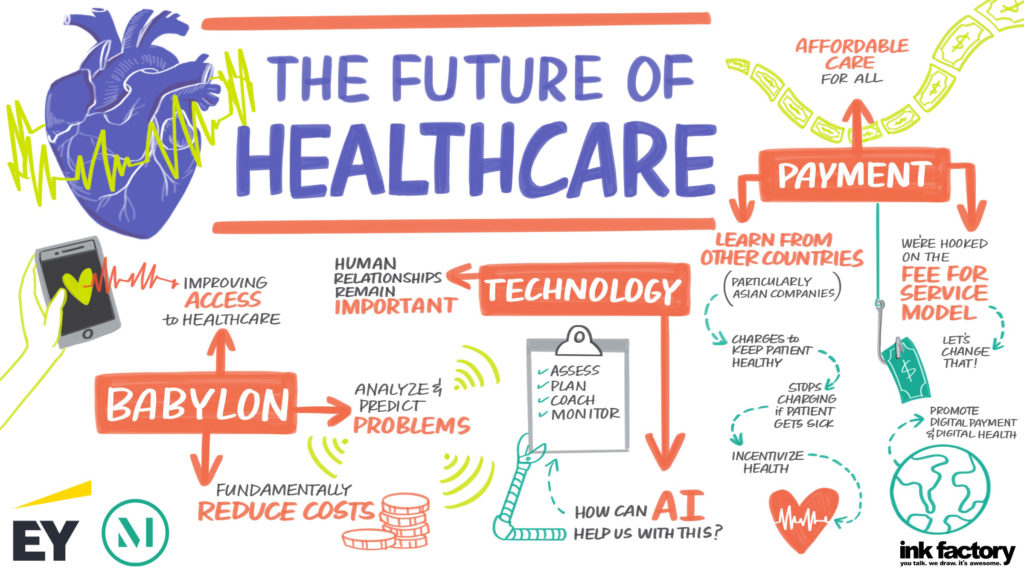
EXPANDING ACCESS TO CARE
Digital health has the potential to make care more accessible. But, for communities without access to technology, we need to figure out how to deliver virtual care. We must ensure emerging technologies do not exacerbate existing health disparities. “The question for (Babylon) was can we do with healthcare what Google did with information: Can we make it accessible and put it in the hands of every human being on Earth? If you think about it, (of) the $10 trillion we spend on healthcare globally, only about 50% of the world’s population (has) any access and about five to seven billion people on our planet actually have no access to any secondary healthcare at all,” Dr. Ali Parsa, chief executive officer at Babylon Health, stated. He continued, “So we sat back and said, accessibility is almost easy because today everybody has a device in their hand, one of these in one format or on their mobile phone, and we can deliver most of the healthcare most people need on the devices. Most people already hav(ing) what could solve the accessibility problem.”
INFORMATION BLOCKING & PATIENT TRUST
One of the critical challenges for digital health is the gap between the promise of the technology and the level of trust consumers have in the technology sector. “We have to actually solve this problem for digital health to advance, and that’s a goal of the digital health industry because consumers do not trust what the industry is doing with their data,” Lucia Savage, chief privacy and regulatory officer at Omada Health, said. She continues, “As a privacy officer answering questions from not only our actual members but people who are interested in our program and want to know how it works, it’s a combination of regularly regulation but also more protection for the user against adverse effects of having that data flowing around the system, maybe more protection against discrimination, etc. And so that’s something that people should really look at, but the industry has to speak up on this because the trust has to be inherent.”
ACCESSIBILITY AND AFFORDABILITY
Two of the biggest problems in healthcare are accessibility and affordability. Digital health has the potential to make healthcare accessible and affordable for all. “In cases where communities don’t have the technology, we need to figure out how we deliver that care,” BJ Moore stated. They may not have reliable internet access, so when we talk about care delivery at home, we’re talking about 5G in a box. So not only sending them home with a smart thermometer and pulse oximeter but sending them home with a 5G hotspot that makes sure that they have internet access to receive that care. In return, they get better health and therefore it’s lower cost to serve those communities. So we definitely see there’s more work to be done, but we see technology already helping us serve those communities. And then you’ll see us investing in those communities to ultimately improve their health outcomes and reduce the cost of care delivery.”
MOVING BEYOND FEE-FOR-SERVICE
The fee-for-service reimbursement model is a fundamental problem in our healthcare system. We need to support alternative systems that inject quality into healthcare delivery. “So there is nothing radical about saying that the payment model in healthcare (is) fundamentally wrong and we should fix it. It’s actually an insane way of doing it. It’s just normal, should be done this way and I think both providers, payors, everybody will benefit from the challenges. Everyone is hooked on this fee-for-service model, the whole system, and yet nobody has got the courage to change the system,” Dr. Ali Parsa said.
ON-DEMAND DIGITAL INTERVENTIONS FOR 2021
The wide adoption of digital tools has an increasing demand in healthcare and creating digital interventions are at the forefront of being developed and analyzed. The impact of digital health innovations can change the trajectory of communities and grows the cost-effectiveness of interventions by reaching a community quicker through content and delivery. “I have my eye squarely on rural underserved communities and disparities because I think that with the data science and the delivery, it’s really a phenomenal opportunity,” said Lucia Savage. “An example will be a model where Omada participated in a Medicaid pilot in Maryland of a diabetes prevention program (DPP). We were in a bake-off with an in-person DPP and Medicaid participants preferred Omada (Health) two to one. You know why? Because they could read a lesson on the bus, on their way to work in the morning or taking their kids (to school). Our members didn’t have to rearrange their lives to go to a particular place in the middle of the week, and that is a really important object lesson. The second thing on the delivery front is protocols that can be delivered outside of the building. Sean Duffy has a great article in New England Journal from three years ago called, ‘When the Hospital is Option B,’ but it’s about digital health’s ability to provide or support a person arranging for themselves relevant health improving protocols outside of the building.”
To catch up on all of the sessions at the McDermott Will & Emery and EY during the 2021 J.P. Morgan Healthcare Conference, please click here.